Dealing with Yeast Infections in Pet Ears

Understanding the Symptoms
Yeast infections, often characterized by vaginal discomfort, can manifest in various ways. Identifying the specific symptoms is crucial for accurate diagnosis and effective treatment. Common symptoms include itching, redness, and swelling of the vulva and vaginal area. A thick, white, cheesy discharge is another typical sign, though the discharge can sometimes be clear or watery. It's important to note that these symptoms can overlap with other conditions, making proper diagnosis essential.
Some women may experience pain during urination or sexual intercourse. These symptoms can range from mild to severe, and their intensity can vary from person to person. It's also important to be aware of any unusual odor associated with the discharge, as this could also be a sign of an infection or other underlying issue. Accurate symptom recognition is the first step in seeking appropriate medical advice.
Factors Contributing to Yeast Infections
Several factors can contribute to the development of yeast infections, ranging from lifestyle choices to underlying health conditions. Diet plays a significant role, with excessive sugar consumption potentially providing a breeding ground for yeast overgrowth. Certain medications, such as antibiotics, can disrupt the natural balance of vaginal flora, increasing the risk of infection. Furthermore, stress, hormonal fluctuations (particularly during pregnancy or menstruation), and weakened immune systems can all contribute to yeast overgrowth. Understanding these contributing factors can help individuals take preventative measures.
Wearing tight-fitting clothing, especially underwear, can also increase the risk of yeast infection. This is because tight clothing traps heat and moisture, creating an ideal environment for yeast to thrive. This is particularly important to consider for individuals who engage in activities that cause them to sweat frequently. Regular hygiene practices and choosing breathable clothing can help mitigate this risk.
Importance of Accurate Diagnosis
Accurate diagnosis is paramount in ensuring appropriate treatment for yeast infections. Self-treating, without a proper diagnosis, can lead to complications or delay effective treatment. If you suspect you may have a yeast infection, it's essential to consult a healthcare professional for a proper evaluation. They can perform a physical examination and may order tests to rule out other potential conditions that may have similar symptoms.
A healthcare provider can accurately determine if the symptoms are indeed caused by a yeast infection or another condition. This ensures that you receive the most effective treatment plan, tailored to your specific needs. Delaying diagnosis can exacerbate the infection or lead to complications, highlighting the importance of seeking professional medical advice.
Treatment Options and Prevention
Effective treatment options for yeast infections typically involve antifungal medications, which can be administered orally or topically. Over-the-counter antifungal creams and suppositories are often effective for mild cases. It's crucial to follow the prescribed dosage and duration of treatment to ensure complete eradication of the infection. Incomplete treatment can lead to recurrence.
Maintaining good hygiene and avoiding factors that contribute to yeast overgrowth are crucial for preventing future infections. This includes wearing breathable clothing, avoiding tight-fitting underwear, and maintaining a healthy diet. Understanding your own body and the factors that may trigger yeast infections can help you take proactive steps towards prevention.
Artificial intelligence (AI) is revolutionizing various industries, and route planning is no exception. By leveraging AI algorithms, businesses can significantly improve their route optimization strategies, leading to substantial cost savings and enhanced efficiency. AI-powered route planning tools analyze vast amounts of real-time data, including traffic conditions, weather patterns, and delivery schedules, to dynamically adjust routes in real-time, ensuring optimal delivery times and minimizing fuel consumption.
Effective Treatment Options for Pet Ear Yeast Infections

Pharmacological Interventions
Pharmacological treatments for acne are designed to target the underlying mechanisms contributing to the condition. These treatments often involve topical medications, such as retinoids, antibiotics, and benzoyl peroxide, which work to reduce inflammation, control bacteria, and regulate oil production. Topical retinoids, in particular, are often considered a cornerstone of acne treatment due to their ability to exfoliate the skin and unclog pores. They can also promote collagen production, leading to improved skin texture and appearance over time.
Oral medications, such as antibiotics and birth control pills, might be necessary in certain cases, especially for severe or cystic acne. These options can help manage inflammation and bacterial overgrowth, but they often come with potential side effects that should be carefully considered with a healthcare provider.
Lifestyle Modifications
While pharmacological interventions are crucial, lifestyle modifications play a significant role in managing and preventing acne breakouts. Maintaining a balanced diet rich in fruits, vegetables, and lean proteins, while limiting processed foods and sugary drinks, can contribute to overall health and potentially reduce acne severity. Proper hydration is also essential for maintaining healthy skin and overall well-being.
Stress management techniques, such as regular exercise, yoga, or meditation, can also have a positive impact on acne. Chronic stress can exacerbate acne, and incorporating stress-reducing activities into your routine can help regulate hormones and improve skin health.
Topical Treatments
Topical treatments offer a localized approach to acne management. These treatments directly target the affected areas, minimizing potential systemic side effects often associated with oral medications. Different topical agents work in various ways, such as targeting bacteria, reducing inflammation, or regulating sebum production. Many topical treatments are available over-the-counter, offering accessibility for individuals seeking simple and effective solutions.
Benzoyl peroxide, for example, is a common over-the-counter acne treatment that works by killing bacteria on the skin's surface. Salicylic acid and glycolic acid are other effective ingredients that exfoliate the skin, improving pore size and reducing the appearance of breakouts.
Professional Skin Care
Professional skin care treatments offer advanced techniques for addressing acne and its underlying causes. These therapies often involve specialized procedures performed by dermatologists or estheticians. Chemical peels, for example, can effectively remove damaged skin cells and unclog pores, leading to smoother and clearer skin. Microdermabrasion is another option that gently exfoliates the skin's surface, reducing the appearance of scars and promoting healthier skin cell turnover.
Surgical Procedures
In cases of severe acne or acne scarring, surgical procedures may be considered as a treatment option. These procedures, often performed by dermatologists, aim to address the underlying causes of acne and reduce the appearance of scars. Surgical treatments may include laser therapy or other advanced techniques to target specific skin concerns. The decision to pursue surgical interventions is a careful one, often made in consultation with a dermatologist, weighing the potential benefits against the risks.
Complementary Therapies
Complementary therapies, such as dietary supplements and herbal remedies, are gaining popularity as part of an overall acne management strategy. However, it's crucial to approach these therapies with caution and in conjunction with a healthcare professional's guidance. Many of these therapies lack rigorous scientific evidence to support their effectiveness and safety. It's important to consult with a dermatologist before incorporating any alternative therapies into your acne treatment plan. While some individuals may find certain complementary therapies helpful, their efficacy in treating acne is not universally established.
Read more about Dealing with Yeast Infections in Pet Ears
Hot Recommendations
- Best Pet Bowls: Stainless Steel and Ceramic
- Pet Hydration: Why It's Crucial
- Stop Counter Surfing: Training Your Dog to Stay Off
- Pet Hypothyroidism: Symptoms and Management
- Signs of Pet Liver Disease: What to Watch For
- Pet Emergency Kits: What to Pack
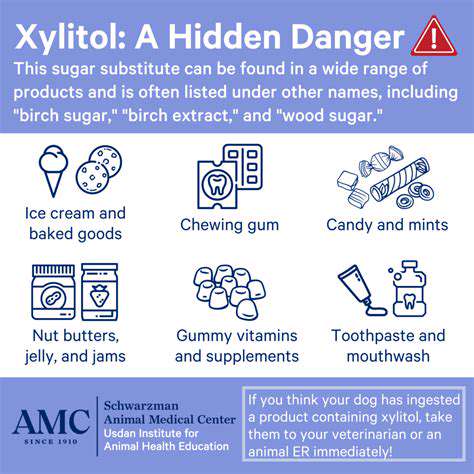
- Dangers of Xylitol: Toxic to Dogs
- Dealing with Pet Diarrhea: When to See a Vet
- Preparing Pets for Travel: Tips for a Smooth Trip
- Pet Depression: Recognizing the Signs