Dangers of Rat Poison: Emergency Protocol
Regulatory differences create geographic variations in available poisons - what's banned in Europe may be common in American hardware stores. Smart homeowners research their local rodenticide landscape before considering any pest control measures.
Symptoms of Rat Poison Exposure
Blood-thinning poisons manifest through telltale hemorrhaging - bloody noses, hematomas under the skin, or blood in urine. Neurotoxic types trigger seizures, tremors, and paralysis starting in the hind limbs. The most insidious cases show only vague malaise for days before sudden collapse. Watch for pale gums, labored breathing, or unexplained bruising as these signal internal bleeding.
Time becomes the critical factor with anticoagulant exposure. Even asymptomatic pets need immediate veterinary evaluation if ingestion is suspected, as the antidote (vitamin K1) works preventatively but can't reverse organ damage once bleeding begins.
Routes of Exposure
Rodents often carry poisoned bait to unexpected locations, creating secondary exposure risks. A dog may find a dying mouse in the yard, or a cat could ingest poison while grooming contaminated paws. Bait stations designed to protect pets sometimes fail when determined animals chew through plastic casings.
Children face particular danger from brightly colored bait pellets resembling candy. Always assume any missing bait was moved by animals rather than consumed at the placement site. The safest approach involves professional extermination with precise placement and monitoring.
Prevention and Safety Measures
Modern pest control emphasizes exclusion techniques over poison use. Sealing entry points with steel wool and maintaining clean spaces proves more effective long-term than toxic baits. When poisons become necessary, choose tamper-resistant bait stations secured with screw-type fasteners.
Store rodenticides in locked cabinets separate from human or pet food. Dispose of unused poison through hazardous waste programs - never in household trash where animals might access it. Consider electronic traps or catch-and-release alternatives for humane, poison-free rodent control.
Symptoms of Rat Poisoning: Recognizing the Signs
Early Warning Signs
The initial indicators often mimic less serious conditions, making poisoning cases frequently misdiagnosed. Affected animals may show slight hesitation before eating or lose interest in favorite treats. Owners report their pets seeming off - perhaps sleeping more or responding slower to commands. These subtle changes warrant immediate investigation when rodenticides are present in the environment.
Digestive System Reactions
As toxins circulate, vomiting episodes may contain telltale bait fragments or blood. Diarrhea often appears black and tarry from digested blood. The abdomen becomes painful to touch as internal bleeding strains organ tissues. Unlike food poisoning, these gastrointestinal signs typically worsen progressively rather than improving with time.
Neurological Impact
Bromethalin exposure causes a distinct set of neurological symptoms beginning with hind limb weakness. Pets may drag their back paws or have trouble jumping onto furniture. As the toxin spreads, uncontrolled muscle twitches progress to full convulsions. Unlike epileptic seizures, these episodes don't respond to standard anti-convulsant medications.
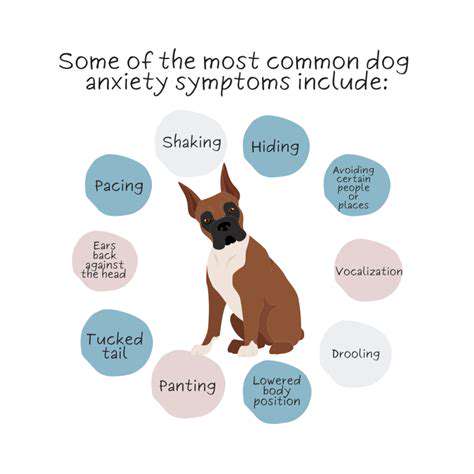
Behavioral Shifts
Poisoned animals often seek isolation, hiding in closets or under beds. Some display uncharacteristic aggression when approached, while others become excessively clingy. These behavior changes reflect the body's distress signals as multiple systems begin failing. Watch for unusual vocalizations or repetitive motions indicating neurological impairment.
Physical Coordination Loss
The poisoning progression typically includes a drunken gait, head tilting, and inability to stand. These symptoms indicate advanced neurological damage requiring intensive care. Pets may circle endlessly or press their heads against walls due to disorientation and headache-like pain from brain swelling.
Terminal Stages
Without intervention, the final hours involve coma, respiratory failure, and uncontrollable bleeding. Different poisons follow different timelines - anticoagulants may take days while neurotoxins kill within 24 hours. Emergency clinics report the highest survival rates when treatment begins before obvious symptoms appear.
Emergency Procedures for Rat Poison Exposure
Critical First Steps
When facing potential poisoning, speed and accuracy save lives. Immediately confine the victim to prevent further toxin absorption through activity. Gather the poison packaging - the EPA registration number helps poison control identify the exact formulation. Never induce vomiting without professional guidance, as some poisons cause more damage coming back up.
If the patient loses consciousness, check for breathing and pulse every two minutes. Position them on their left side to slow toxin absorption and prevent aspiration. Cover with a blanket to combat shock while awaiting emergency responders.
Identifying the Toxin
The treatment protocol varies dramatically by active ingredient. Anticoagulants require vitamin K supplementation, while bromethalin has no antidote and needs aggressive decontamination. Even bait packaging fragments help toxicologists determine the chemical class and appropriate response.
Photograph any remaining bait or vomited material for veterinary reference. Note the estimated amount missing and approximate ingestion time. These details guide treatment intensity and duration.
Medical Intervention
Emergency clinics typically administer activated charcoal to absorb intestinal toxins, followed by blood tests assessing clotting function and organ values. Hospitalization allows intravenous fluids to support kidney function and medications to control symptoms. Severe cases may require plasma transfusions to replace clotting factors.
Follow-up care often spans weeks for anticoagulant cases, with periodic blood monitoring to ensure proper clotting function has returned. Owners should prepare for substantial medical costs - comprehensive poisoning treatment frequently exceeds $2,000.
Environmental Cleanup
After securing medical care, eliminate remaining poison hazards. Wear nitrile gloves when collecting bait remnants and contaminated materials. Hard surfaces require scrubbing with detergent, while porous materials may need replacement. The EPA recommends specific disposal methods for rodenticides to prevent ecosystem contamination.
Long-Term Health Monitoring
Survivors often experience lasting effects depending on the toxin type and exposure duration. Anticoagulants may cause permanent liver impairment, while neurotoxins can leave residual tremors or cognitive changes. Schedule biannual veterinary checkups to catch late-developing complications early.
Behavioral rehabilitation helps pets regain confidence after traumatic poisoning events. Be patient with housetraining regression or new anxieties that may emerge during recovery.
Recent neurology studies reveal inflammation's complex role in migraine pathology, with cytokine pathways offering new treatment targets. Emerging monoclonal antibodies that block calcitonin gene-related peptide (CGRP) demonstrate particular effectiveness for chronic migraine sufferers. Ongoing glial cell research may yield drugs that modulate neuroinflammation without suppressing the entire immune system.
First Aid and Medical Treatment

Essential First Aid Knowledge
Proper first aid application bridges the gap between incident and professional care. Correct technique application often determines whether injuries heal completely or develop complications. These skills prove particularly valuable in remote areas where emergency response times exceed golden hour windows.
Regular refresher courses maintain readiness, as protocols evolve with medical advancements. Focus on mastering bleeding control, fracture stabilization, and poisoning response - the three most common pet emergencies requiring first aid.
Situational Awareness
Effective responders first eliminate ongoing dangers - downed power lines, aggressive animals, or chemical spills. Use available resources creatively; a belt becomes a tourniquet, newspapers make splints, and plastic bags serve as makeshift gloves. The priority sequence always remains: ensure safety, assess responsiveness, then administer care.
Quickly evaluate breathing quality, pulse strength, and consciousness level. Note any wounds, swellings, or abnormal postures before touching the patient to avoid exacerbating injuries.
Wound Management
Control bleeding with firm pressure using the cleanest available material. For severe hemorrhage, consider pressure points above the wound or a carefully placed tourniquet. Remember that wound irrigation matters more than antiseptics - copious clean water flushing removes debris and bacteria.
Leave impaled objects in place unless obstructing airways. Stabilize them with bulky dressings to prevent movement during transport. Deep puncture wounds always require veterinary evaluation due to infection risks.
Shock Recognition
The shock triad - rapid pulse, pale gums, and delayed capillary refill - signals circulatory collapse. Keep the patient warm with blankets but avoid direct heat sources. Elevate the hindquarters slightly unless spinal injury is suspected. Quiet, calm handling prevents further stress to the compromised system.
Monitor respiratory rate and mental status changes every five minutes. Document these observations for veterinary staff to identify deterioration trends.
Emergency Transport
Stabilize fractures with makeshift splints before moving the patient. Use rigid materials like magazines or boards padded with clothing. For spinal injuries, slide the animal onto a flat surface without bending the spine. Muzzle painful patients to protect responders, using gauze or fabric strips if no proper muzzle is available.
Call the receiving clinic during transport to prepare the staff. Provide concise information: patient status, suspected injuries, and estimated arrival time.